By J. C. Trussell, MD
 Infertility affects 6.1 million U.S. couples — representing 10 percent of reproductive aged adults or 15 percent of all couples trying to conceive. Over the past decade, there has been a steady increase in the number of couples seeking fertility assistance. Medically it is important that both the male and female partner to be evaluated. For the male, this involves a brief history and physical exam, including a semen analysis.
Infertility affects 6.1 million U.S. couples — representing 10 percent of reproductive aged adults or 15 percent of all couples trying to conceive. Over the past decade, there has been a steady increase in the number of couples seeking fertility assistance. Medically it is important that both the male and female partner to be evaluated. For the male, this involves a brief history and physical exam, including a semen analysis.
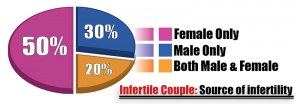
Unfortunately, half of the time, a male cause for infertility is discovered — 20 percent of the time there will be a concurrent female infertility factor, while the remaining 30 percent of men will be the sole cause for infertility [Figure 1].

Again, male factor infertility is common; it is therefore imperative that both the male and female undergo a medical evaluation.
In the absence of a clear medical or surgical condition (such as a vasectomy or a genetic condition), men are classified as having “idiopathic infertility.” After a complete workup, this is the diagnosis up to 50 percent of the time. Such men continue to have treatment options, with a recent survey reported that two-thirds of responding U.S. urologists would use empiric (off-label) therapies to treat men with idiopathic male factor infertility. The most commonly used medications are clomiphene citrate (Clomid), human chorionic gonadotropin (hCG), and, anastrozole/letrozole.
In fact, a recent review of pooled data from four randomized, controlled trials using gonadotropins (hCG), demonstrated an improved pregnancy rate (13.4 percent versus 4.4 percent for those not being treated).
Off-label therapies
Clomiphene Citrate (Clomid) is an oral medication that works by tricking the brain to release more chemical to stimulate the testes — like putting high-octane fuel into the testes’ gas tank. Not everyone responds the same to Clomid. For this reason, it is imperative that clients on Clomid are carefully monitored to verify semen analysis improvement. When defining an adequate Clomid response as a “pregnancy” or a 100 percent improvement in total motile sperm count, more than 50 percent of patients (35 of 53 subjects) responded by three months. The remainder will take six to 15 months to respond. For this reason, it may take a year or more to realize improved semen parameters. Having said that, based on current evidence, it appears that Clomid may be effective in treating most cases of idiopathic male factor infertility.
Human Chorionic Gonadotropin (hCG) shots are indicated in men whose brain is not making “gas” to stimulate the testicles. hCG is a shot you give yourself three times a week, to replace the “gas” missing from the brain. This hCG replacement is like adding an accessory (or back up) fuel tank to a motor. The testis stimulation will only occur while the hCG shots are being administered.
Anastrozole and Letrozole are prescription medications that belong to a class of aromatase inhibitors (AIs). Aromatases are a normal part of abdominal fat cells, which facilitate the breakdown of testosterone to another hormone called estradiol. Both testosterone and estradiol travel to the brain and turn off the brain’s production of “gas.” Less “gas” to stimulate the testes will result in lower sperm production. AIs block the aromatase enzyme, resulting in less inhibition of the brain’s “gas” production — resulting in greater testicular sperm production. A simple blood test is used to determine if a client would likely respond to AIs treatment. Treating men with AIs is associated with both improved sperm concentrations (from 5.5 to 15.6 million sperm/mL) and, increased testosterone levels.
Testosterone replacement must be avoided. Testosterone is essential for the development of male reproductive organs (penis, prostate, seminal vesicles, vas deferens and epididymis) and for subsequent puberty, sexual function, and fertility. Exogenous testosterone (gels, injections) will wipe out the brain’s “gas” production — resulting in a severe drop in sperm production. Unfortunately, stopping exogenous testosterone replacement does not guarantee return of sperm production. Only 65 percent of men will recover sperm production 6 months after discontinuing T-replacement.
Treating the 50 percent of men with idiopathic infertility is a vexing problem. Treatment options include therapies such as Clomid, hCG, and/or Anastrazole/Letrozole. Careful follow up is necessary to be sure that the expected semen parameter improvement is realized.
Author’s note: Adapted from: Mahmoud Chehab, Alosh Madala, JC Trussell. “On-label and off-label drugs used in the treatment of male infertility.” Fert Steril 2015;103:595-604.
