That’s a common condition affecting women but about 25% of men will experience a bone break associated with osteoporosis
By Deborah Jeanne Sergeant
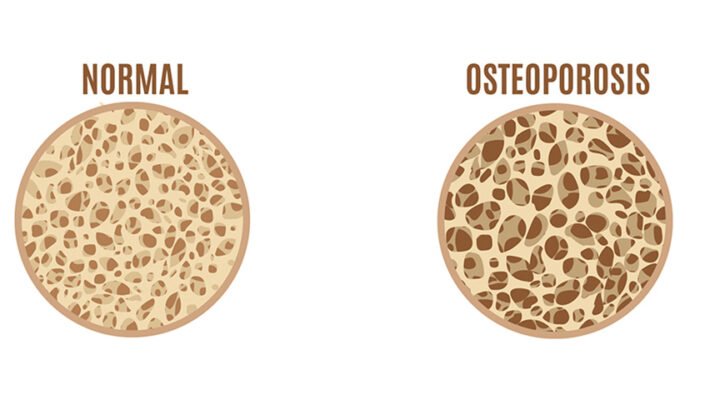
Osteoporosis is an often-overlooked health concern for men.
About 25% of men older than 50 will experience a bone break associated with osteoporosis. About 20% of osteoporosis cases are men, but their hip fractures account for almost 30% of hip fractures. Overall, men’s long-term osteoporosis outcomes are worse.

One of the reasons that men—and their care providers—do not think about osteoporosis is that its effects are not as apparent as with women.
“Men start out with bigger bones,” said Susan Brown, Ph.D., of Center for Better Bones in East Syracuse. “You don’t see the bone loss as quickly.”
Brown is a medical anthropologist, certified nutritionist and author of Better Bones, Better Body.
She also said that men are not necessarily seeking bone density testing because their risk is perceived as small because of their heavier frames. This does not account for higher male risk factors, such as greater prevalence of smoking (17.5% of men vs. 13.5% of women, states the American Lung Association), drinking alcohol in excess (men are twice as likely to binge drink, states the Centers for Disease Control and Prevention) and use of certain bone-weakening medication such as proton pump inhibitors and prednisone (although both genders take these medications at the same rates, women usually take lower doses sooner compared with men, according to the National Institutes of Health.).
Men typically learn about their osteoporosis as a secondary diagnosis, usually after a fracture or because of low testosterone testing and not as part of a routine work-up.
While most men have a larger frame than most women—a protective factor for guys—those men with a lighter body weight and smaller frame have a higher risk for lower bone density.
Genetics also matters
“Look at your family history,” Brown said. “If you have a history where a man’s father had fractures, what prescriptions did they use? What was their diet like? You could have genetic quirks like vitamin D metabolizing.”
For those with higher risk factors, mitigating those risks is essential for preventing osteoporosis and debilitating bone breaks.
Brown looks at the overall diet—and not just about consuming foods containing calcium. Foods rich in minerals such as magnesium, found in nuts and seeds, and vitamin C, inherent to citrus fruits, tomatoes and many other fruits and vegetables, help keep bones strong, along with other nutrients. Vitamin D, the “sunshine vitamin” also makes a difference. It takes moderate weekly sun exposure or supplementation to get enough as few foods contain D vitamin naturally. To ensure the body absorbs nutrients, Brown promotes an alkaline diet, which emphasizes eating eight to 10 cups (pre-cooking) of vegetables daily and eschewing processed, empty-calorie foods.
“One-third of people in New York don’t eat one fruit or vegetable daily,” Brown said. “They have the calories in their diet but not the nutrients.”
For a “meat-and-potatoes” man, making dietary changes can be tough. However, incorporating more veggie-based meals in the week can help improve the diet, such as chicken taco salad.
Maintaining muscle mass can also help protect bones. As people age, they tend to lose muscle and bone. Diminishing fitness can also include reduced sense of balance and less flexibility, which can contribute to falls. To prevent this cascade toward deconditioning, Brown stressed the importance of strength training and weight-bearing exercise.
She also encourages people to manage their stress.
“Surprisingly, stress damages bone,” she said. “It’s very important to recognize you’re stressed and worried and take time to have silent walks in the woods and meditate. You can nourish the nervous symptom in quiet.”
Brown offers a library of bone health information and screening tools at www.betterbones.com.
Julie Mellen, registered dietitian with Upstate University Hospital, encourages patients to meet their calcium needs through three servings of calcium-rich foods daily.
“Milk, yogurt, cheese, kale and other dark, leafy greens provide calcium,” Mellen said. “Nondairy fortified products like almond milk that has calcium and vitamin D added to it can also help.”
For those who do not consume calcium-rich foods, “a supplement would be good,” she added.